Cultural Competency and Its Effect on Treatment Outcome of IPT-A in School-Based Health Clinics
Abstract
Background: This paper assesses acculturation and ethnic matching of therapist and patient as predictors and moderators of treatment outcome in a 12-week effectiveness study of Interpersonal Psychotherapy for depressed adolescents (IPT-A) versus treatment as usual (TAU). The treatment was delivered in school-based health clinics in which care was provided for a predominantly Latino patient population.
Methods: Birthplace, length of residence in the United States (U.S.), and therapist-patient ethnic matching were examined as predictors and moderators of treatment outcomes for depression, social functioning, and global functioning scores.
Results: Birthplace significantly moderated treatment condition in predicting week 12 depression severity and improvement, and marginally significantly moderated treatment in predicting week 12 depression symptoms, with U.S.-born adolescents who received IPT-A having better outcomes. Birthplace predicted week 12 self-reports of depression, social (overall, school, and family) and global functioning, with U.S.-born adolescents faring worse across treatment conditions. Foreign-born adolescents treated with IPT-A as compared to TAU who lived for a longer period of time in the U.S. demonstrated better overall social functioning as compared to foreign-born adolescents who had lived for a shorter period of time in the U.S. Ethnic matching predicted significant reduction in depression severity and improved overall social functioning, and marginally significant improvement in week 12 depression scores, regardless of treatment condition.
Conclusions: IPT-A may be a culturally responsive treatment for depressed Latino youth who are struggling with acculturation issues that affect their significant relationships. Ethnic matching appears beneficial for the general population in reducing depression and improving social functioning.
Introduction
Research has focused on identifying empirically supported treatments (ESTs) for particular disorders, and has paid less attention to the cultural competency of those interventions (Bernal & Sharrón-del-Río, 2001). However, as these treatments move from the university setting to the outside community, the importance of cultural competency is being re-emphasized. The effectiveness of ESTs appears less robust in community settings in which heterogeneous and minority populations are being treated (Weersing & Weisz, 2002; Weisz et al., 2013). Studies show that mental health services, especially empirically supported psychotherapies, have not been available and/or effectively delivered to minority populations (Bernal & Sharrón-del-Río, 2001; Hall, 2001; Sue & Zane, 2006; Markowitz, Spielman, Sullivan, & Fishman, 2000). The growth of minority populations—particularly the Latino population, which (along with the Asian population) grew the fastest in the last decade (U.S. Census Bureau, 2010)—will continue to limit the relevance of efficacy trials for treatments unless their effectiveness with these populations can be demonstrated.
Despite the need to ensure treatment effectiveness for minority populations, how researchers should proceed to address this issue is unclear. Lau (2006) suggested using cultural adaptations of treatments if the problems the individual encounters are influenced by membership in a particular community or if members of that community respond poorly to a standard EST. However, few ESTs have been formally tested with or without adaptations for minority groups, such as Latinos (Bernal & Sharrón-del-Río, 2001; Huey & Polo, 2008).
It is possible that interventions that have not been adapted for specific cultures may contain features that make them well-suited to these cultural groups. For example, Rosselló and Bernal (1999) reported that the focus on current interpersonal conflicts make Interpersonal Psychotherapy (IPT) a culturally acceptable treatment to Latinos because of its relevance to Latino values of familismo and personalismo. Familismo refers to Latino culture’s emphasis on the importance of the family’s well-being over one’s individual needs and of connectedness to one’s family. Personalismo refers to the desiring and valuing of personal relationships with others (Añez, Paris, Bedregal, Davidson, & Grilo, 2005). With IPT’s emphasis on restoring harmony to one’s relationships, both familial and peer, IPT may help Latino patients feel that their values are respected and incorporated into the goals of treatment without requiring additional cultural adaptations. The culturally competent clinician would modify the style of communication to be more syntonic with cultural norms for conducting relationships and explore new ways of communicating that might be helpful in achieving improved relationships (Markowitz et al., 2009).
Determining Cultural Competency: Therapist-Related Factors
Cultural competence is embedded in multiple aspects of an intervention, including the clinician’s ability to deliver the treatment in the patient’s preferred language, the clinician’s interpersonal style in delivering the intervention, and the clinician’s ability to provide a cultural context for the intervention (Andrés-Hyman, Ortiz, Añez, Paris, & Davidson, 2006). One way that this concept has been examined is through ethnic matching of client and therapist.
Therapists who share their patients’ ethnic backgrounds are more likely to have similar cultural backgrounds, which helps to facilitate the provision of culturally responsive treatment (Sue, Fujino, Hu, Takeuchi, & Zane, 1991; Tharp, 1991). Ethnic matching appears to reduce the likelihood of miscommunication between patient and therapist stemming from cultural differences (Sue, 1998), which may increase patient self-disclosure and empathy (Fiorentine & Hillhouse, 1999) and reduce clinician ethnic biases (Halliday-Boykins, Schoenwald, & Letourneau, 2005). Fuertes and colleagues (2006) found that minority ethnic patients who rated their therapists more multi-culturally competent also rated them highly on measures of therapeutic alliance and empathy. Therefore, cultural competency is intertwined with general perceptions of the therapist-patient relationship. Additionally, studies have consistently shown that ethnic minority clients prefer an ethnically similar counselor over an ethnically dissimilar counselor (Proctor & Rosen, 1981; Terrell & Terrell, 1984; Watkins & Terrell, 1988; Watkins, Terrell, Miller, & Terrell, 1989).
Studies examining the effects of ethnic matching on treatment outcome are relatively rare (Hall, 2001) and have primarily been conducted with adults receiving usual care in community settings (Erdur, Rude, & Baron, 2003; Fiorentine & Hillhouse, 1999; Sue et al., 1991). Only a few studies have focused on these effects with children and adolescents (Hall, Guterman, Lee, & Little, 2002; Jerrell, 1998; Yeh et al., 1994). The available findings on treatment outcomes associated with ethnic matching are mixed (Gamst, Dana, Der-Karabetian, & Kramer, 2000, 2004; Sue, 1991; Yeh et al., 1994). However, results generally support the use of ethnic matching with Latino adolescents and adults in community settings (Gamst et al., 2000; Hall et al., 2002; Russell, Fujino, Sue, Cheung, & Snowden, 1996; Sue et al., 1991; Yeh et al., 1994). Specifically, adolescent and adult studies have found that ethnically matched Latino clients tend to drop out less frequently from treatment and attend more sessions (Hall et al., 2002; O’Sullivan & Lasso, 1992; Yeh et al., 1994). The impact of ethnic matching on the implementation of empirically supported psychotherapies, such as Interpersonal Psychotherapy with Latino adolescents, has not been examined to date.
Determining Cultural Competency: Patient-Related Factors
Although intervention-related factors are paramount in determining its cultural competency, the importance of these factors for treatment outcome may vary by the patient’s level of acculturation and assimilation. Acculturation refers to the sociocultural change process that individuals experience when encountering and adapting to a new culture (Berry, Phinney, Sam, & Vedder, 2006; Williams & Berry, 1991; Lopez-Class, Castro, & Ramirez, 2011). This may entail assuming the values, language, and cultural practices of the host society or undergoing changes in language, socioeconomic status and/or cultural orientation such as alterations in values and attitudes (Olmedo, 1979). Researchers have identified two components of the acculturation process: 1) culture of origin involvement (enculturation) and 2) host cultural involvement (assimilation), and recognize their effects on mental health in immigrants (Gonzales, Knight, Morgan-Lopez, Saenz, & Sirolli, 2002).
Some of the changes inherent in the acculturation process can be stressful, including family separations and reunifications, trauma before and during the journey, change in socioeconomic status, and changes in family rules and roles (Portes & Rumbaut, 2001). Adolescents may be particularly susceptible to the effects of stressors during the acculturation process. Acculturative stress during adolescence may lead to increased conflict with parents, which may intensify typical adolescent struggles with developmental changes, identity conflicts, individuation, and autonomy. Adolescents tend to adopt the language, values, and behaviors of the dominant culture more easily than their parents, which may result in a clash with the parents’ traditional values and behaviors (Portes & Rumbaut, 2001). As a result, adolescents may become more immersed within mainstream culture of the United States (U.S.; more assimilated) than their more enculturated parents (Fulgini, 1998), creating a gap and concomitant tension between the acculturation levels of adolescents and their parents (Pasch et al., 2006).
Although adolescents may assimilate more quickly than their parents, research has shown that, for Latino adolescents, both high and low levels of acculturation may be risk factors for various problems, including depression (Gonzales, Knight, Birman, & Sirolli, 2004; Hovey & King, 1996), substance abuse (Brook et al., 1998), poor school functioning (Chapman & Perreira, 2005; Vega, Khoury, Zimmerman, Gil, & Warheit, 1995), and delinquent behavior (Fridrich & Flannery, 1995; Gonzales et al., 2002). Gonzales and colleagues (2002) reviewed 10 studies assessing acculturation and adolescent aggression, finding that 6 of the 8 adolescent studies reported that higher assimilation was associated with greater delinquency and stronger relationships with antisocial peers. In contrast, Glover, Pumariega, Holzer, Wise and Rodriguez (1999) found that foreign birth and low English language fluency were significant risk factors for adolescent anxiety in the Latino population. Thus, the effectiveness of a treatment for a Latino patient may depend on how well it addresses acculturation level and associated difficulties.
The emergence of acculturation research has brought about diverse and changing views of the acculturation process, which influence how acculturation is measured. Early on, acculturation typically was measured by single items, such as place of birth or language predominantly spoken in the home and other proxy measures, for example, generational status and age at migration (Lopez-Class et al., 2011). More recently, however, the definition of the acculturation process has expanded to include concepts such as changes in attitudes and values, and recognition that the process is influenced by the context in which it occurs. For these reasons, other measures of acculturation were developed to capture changes occurring on multiple dimensions, including beliefs, values, attitudes, and behaviors (Thomson & Hoffman-Goetz, 2009). Extant measures examine the presence of racial or ethnic discrimination and the effects of the acculturation process on personal contexts, such as family and socioeconomic status (Lopez-Class et al. 2011, Abraido-Lanza, Armbrister, Florez & Aguirre, 2006). Several well-researched and validated measures include the Acculturation Scale for Mexican Americans II (Cuellar, Arnold, & Gonzalez, 1995), the Bidimensional Acculturation Scale for Hispanics (BAS; Marin & Gamba, 1996), and the Hispanic Stress Inventory (Cervantes, Padilla, & Salgado de Snyder, 1991); however, since this was not initially part of the study design, we will be examining acculturation using proxy measures to obtain a preliminary look at how acculturation may affect Latino adolescents’ mental health and treatment outcomes.
The evidence for the role of acculturative stress in the development of negative outcomes in Latino youth makes it important to examine whether specific interventions may be more effective than others in treating depressed Latino youth who are at varying acculturation levels. Interpersonal Psychotherapy is a time-limited, empirically supported psychotherapy that may be particularly relevant for Latino youth given that the constructs and techniques can encompass and directly address the strains associated with changing family attachments, development of a new social support system, and intergenerational conflict arising from the acculturation process. Interpersonal Psychotherapy is based on the premises that depression occurs in an interpersonal context, depressed mood can affect relationships, and problems in relationships can affect mood. The targeted problem areas of IPT (grief, role transitions, interpersonal role disputes and interpersonal deficits) have demonstrated universality and relevance in diverse cultures (Bolton et al., 2003, 2007; Patel et al., 2010; Markowitz et al, 2009). The adolescent adaptation, IPT-A, has demonstrated effectiveness for depressed adolescents, largely Latino and from underserved communities (Mufson, Weissman, Moreau, & Garfinkel, 1999; Mufson et al., 2004). It remains important to examine whether IPT-A, in its original form, meets the standard of cultural responsiveness and competency for a Latino adolescent population without specific cultural modifications beyond discussions of how to be sensitive to culturally accepted styles of communication between parents and their children.
Although research exists on the effects of level of acculturation and therapist-client ethnic matching, few studies have examined the effects of both these cultural competency factors as predictors and/or moderators of treatment outcomes for an empirically supported psychotherapy such as IPT. Moderators of treatment are patient characteristics present prior to treatment, independent of the type of treatment the patient receives. These have an interactive effect on treatment outcome with the type of treatment received (Kraemer, Wilson, Fairburn, & Agras, 2002). These patient characteristics can also be predictors—characteristics related to treatment outcome, regardless of the type of treatment received (Kraemer et al., 2002).
The current study examined two aspects of cultural competency: 1) the impact of level of acculturation, as determined by the proxy measures of place of birth (foreign or the U.S.) and length of residency in the U.S., and 2) the impact of ethnic matching between therapist and patient as predictors and/or moderators of treatment outcome in a randomized controlled trial of IPT-A compared to treatment as usual (TAU) for Latino adolescents suffering from depression. The impact of place of birth and length of residency on pretreatment levels of depressive symptoms and functioning was also examined. As these acculturation analyses were restricted to a Latino subset of the full sample used in Mufson et al. (2004), this paper attempts to replicate the findings from the original clinical trial sample in the Latino-only sample. These analyses must be considered exploratory in nature as they are post hoc and limited by the use of proxy measures of acculturation. Although this study was exploratory, our a priori hypotheses were: 1) Adolescents who received IPT-A will have better treatment outcomes as measured by the primary outcome measures of depression (Hamilton Rating Scale for Depression, HRSD) and overall functioning (Children’s Global Assessment Scale, CGAS) despite level of acculturation, and 2) those adolescents who received IPT-A and were matched ethnically with their therapists would report better treatment outcomes on the primary measures.
Methods
This paper reports on a secondary data analysis of an effectiveness study titled Interpersonal Psychotherapy for Depressed Adolescents, which was delivered in school-based health clinics (Mufson et al., 2004). Students were assessed at baseline and every four weeks with their clinical status at week 12 the a priori major acute-treatment outcome time point.
Ethnic matching between patient and therapist was examined as a predictor and/or moderator of treatment outcome at week 12 in the overall sample as discussed in Mufson et al. (2004). This sample of adolescents treated with IPT-A displayed significantly greater reductions in depression symptoms and impairment, and significant improvement in social and family functioning at week 12 compared to those who received TAU (Mufson et al., 2004).
The subset of Latino adolescents from the Mufson et al. (2004) study was used to examine acculturation in the present study. The analyses conducted in Mufson et al. (2004) were repeated with this Latino-only subsample to determine if the original results could be replicated in this ethnic subsample. Place of birth (foreign born or in the U.S.) and length of residence in the U.S. were used as acculturation measures and examined as predictors and/or moderators of treatment outcome at week 12.
Participants
Ethnic Matching. Analyses were conducted on an intent-to-treat sample (N=63) of depressed adolescents who participated in the effectiveness study comparing IPT-A (N=34) to TAU (N=29) in a randomized clinical trial. The trial was conducted in five school-based health clinics (three middle schools, two high schools) located in urban, impoverished areas of New York City (Mufson et al., 2004). The sample consisted of adolescents aged 12 to 18 years with a mean age of 15.9 years (SD=1.9). Most (N=47, 74.6%) adolescents were Latino, with the remainder African American (N=9, 14.3%), Asian (N=1, 1.6%), or Other (N=6, 9.5%). Subjects received services from 13 therapists including 11 social workers and two doctoral-level clinical psychologists. The ethnicities of the providers were: 46.2% Caucasian; 46.2% Latino; and 7.7% African American. Therapists were predominantly female (84.6%) and bilingual (76.9%).
Acculturation Analyses. Acculturation analyses were limited to the Latino adolescents (N=50) from the Mufson et al. (2004) full sample. Of this sample, N=28 received IPT-A and N=22 received TAU. This sub-sample consisted of adolescents aged 12 to 19 years with a mean age of 14.6 years (SD=19). Most (N=36; 72%) adolescents were born in the U.S. The remaining individuals in the sample (N=14) were born in Puerto Rico (N=4; 8.0%), the Dominican Republic (N=8; 16%), and Central or South America (N=2; 4%). The sample was predominantly female (N=43; 86%).
All adolescents referred for a mental health intake at the school-based clinics were eligible to be screened for study participation. Study eligibility criteria included a Hamilton Rating Scale for Depression (HRSD, 24 item; Williams, 1988) score of 10 or higher and a Children’s Global Assessment Scale (CGAS; Shaffer et al., 1983) score of 65 or lower at initial clinical intake and at baseline evaluation. Additional requirements were parent consent, adolescent assent, and a baseline DSM-IV diagnosis of major depression, dysthymia, adjustment disorder with depressed mood, or depressive disorder not otherwise specified. Adolescents were excluded if they were actively suicidal or intellectually disabled, had a life-threatening medical illness, met diagnostic criteria for substance abuse disorder, psychosis or schizophrenia, were currently in treatment for depression, or were taking antidepressant medication.
English-speaking students were accepted at all five schools. Two schools accepted monolingual, Spanish-speaking students because both the IPT-A and TAU clinicians were bilingual. (See Mufson et al., 2004, for details including patient eligibility requirements, therapist training and supervision, etc.)
Design Overview
Randomization. Random assignment occurred at both the subject and clinician levels using tables of random numbers. The adolescents were randomly assigned to either IPT-A or TAU at the school-based clinic. Approximately half the clinicians (six social workers and one psychologist) were trained in IPT-A (Mufson et al., 2004).
Treatment. Interpersonal Psychotherapy for adolescents (IPT-A) is a short-term psychotherapy that focuses on current interpersonal problems that may be contributing to or exacerbating the adolescent’s depression. The procedures and techniques of IPT-A are specified in a manual (Mufson, Dorta, Moreau, et al., 2004). Primary objectives of IPT-A include reducing depressive symptoms and improving interpersonal functioning by relating the symptoms to one of four interpersonal problem areas (grief, role disputes, role transitions, and interpersonal deficits) and by learning strategies for addressing these problems. The IPT-A clinician helps the adolescent understand his feelings surrounding the significant relationships and how they influence his behavior in the relationships. Subsequently, the IPT-A clinician teaches the patient communication and problem-solving skills and helps the adolescent apply them to the targeted relationships resulting in decreased depression symptoms. Prior to the effectiveness study, two independent studies had demonstrated the efficacy of IPT-A (Mufson et al., 1999; Rosselló & Bernal, 1999). In the Mufson et al. (2004) effectiveness study, the IPT-A treatment protocol was comprised of 12 sessions occurring over 12 to 16 weeks, with most sessions occurring by the week 12 in-person evaluation timepoint. The TAU condition consisted of the regular psychological treatment adolescents received in the school-based clinic.
Measures. Assessments were conducted by a psychologist or social worker blinded to the subject’s treatment condition. The assessments were conducted at baseline, weeks 4, 8, 12, and 16 or at early termination. A telephone follow-up interview was conducted at week 16. The current and original analyses (Mufson et al., 2004) do not include week-16 assessments because they were conducted by phone and were not full assessment batteries including clinician interviews and self-report measures. Treatment outcome variables for these analyses were assessed at the week 12 time point.
Assessing Depression Symptoms
Hamilton Rating Scale for Depression (HRSD). The 24-item HRSD (Hamilton, 1967; Williams, 1988) is a clinician-administered, semistructured interview assessing the severity of depression symptoms. Scores range from 0 to 74, with a score of 0-7 considered normal and a score greater than 20 considered moderately severe. A score of 10 or greater, suggesting a mild to moderate level of symptomatology, was required for study entrance. Interrater reliability of the HRSD for the current sample was .84, and internal reliability (Cronbach’s alpha) was .74 (α=.81 for the Latino sample).
Beck Depression Inventory (BDI). The BDI is a self-report instrument assessing depressive symptomatology (Beck, Steer, & Garbin, 1988). Its 21 items each allow four ratings of severity ranging from 0 to 3 and a total range of 0 to 63. A BDI score of greater than 15 suggests a likely diagnosis of major depression. The BDI has demonstrated reliability in assessing depression in adolescents (Strober, Green, & Carlson, 1981). Internal consistency in this sample was excellent (alpha=.89). The BDI has been used in previous studies with Latino adolescents (Becker, Kaplan, Tenke, & Tartaglini, 1991; Emslie, Weinberg, Rush, Adams, & Rintelmann, 1990; Mufson et al., 1999; 2004). In the Latino sample, internal reliability (Cronbach’s alpha) was .88.
Global Functioning
Children’s Global Assessment Scale (CGAS).Shaffer et al. (1983) modified the CGAS for use with children. This clinician-rated instrument measures impairment and level of functioning over a one-month interval in all spheres of the child’s life. The scale ranges from 1 to 100 on a hypothetical continuum of health, with 1 representing the lowest level of functioning and 100 the highest. It reliably assesses impairment in children with psychiatric disorders (Shaffer et al., 1983). It has been translated into Spanish and used with a Latino population (Bird, Canino, Rubio-Stipec, & Ribera, 1987).
Clinical Global Impression (CGI). The Clinical Global Impression Scale asks two questions of the clinician: How ill do you feel the patient is (severity), and how improved is the patient (improvement; Guy, 1976). Scores range from 1 to 7 for each question, with lower scores indicating better functioning. The CGI is commonly used in clinical outcome trials to track changes in clinical status.
Social Functioning
Social Adjustment Scale—Self-report (SAS-SR;Weissman, Orvaschel, & Padian, 1980). The SAS-SR, a brief self-report instrument, contains 23 questions in four major categories: school, friends, family, and dating. Patients rate their functioning for the past two weeks on a five-point scale, with higher ratings signifying impairment. Patients receive five scores, one for the total of all scored domains, and one for each individual domain. The SAS-SR has demonstrated sensitivity to change in patients’ clinical status; clinical recovery improves patients’ social adjustment (Weissman & Bothwell, 1976; Weissman, Olfson, Gameroff, Feder, & Fuentes, 2001). Developed for adults, the SAS-SR has been used with adolescents (Garber, Kriss, Koch, & Lindholm 1988; Mufson et al., 1999; 2004); in Latino adolescents, internal consistency was good for the overall scale (alpha=.73; Mufson et al., 1999) and also for the Latino sample (alpha=.82).
Acculturation and Ethnic Matching
Acculturation. There were two measures of acculturation: 1) Birth-place, which was determined by whether or not the adolescent was born in the U.S. (N=14 foreign-born, N=36 born in the U.S.), and 2) for the subset of adolescents who were either born outside of the U.S. (N=14) or who were U.S. born, but had lived abroad (N=4), the number of years an adolescent had lived in the U.S.
Ethnic Matching. An ethnic matching variable (e.g., matched vs. un-matched) measured concordance between the adolescent’s and therapist’s ethnicity.
Data Analysis
Replication of Previous Findings Using Latino-Only Sample
In order to replicate the previous findings from Mufson et al. (2004) with the Latino only sample, analyses of covariance were used to compare treatment conditions controlling for pretreatment levels on each outcome measure.
Acculturation Analyses
T-tests and chi-square analyses were used to examine differences between treatment conditions for the acculturation predictor/moderator variables (i.e., place of birth, years living in the U.S.). Associations between the predictor/moderator variables and pretreatment levels of the outcome measures (i.e., HRSD and BDI depression symptoms, SAS-SR social, school, and family functioning, CGAS global functioning, depression severity and improvement as measured by the CGI) were examined two ways: T-tests were used to examine the association between place of birth and pretreatment depression symptoms and functioning, and a series of linear regressions controlling for age examined the association between number of years adolescents had lived in the U.S. and pretreatment depression symptoms and functioning.
Linear regressions were conducted to examine whether place of birth or years living in the U.S. moderated treatment outcome. This included testing the interaction between treatment condition (IPT-A vs. TAU) and each predictor on treatment outcome, controlling for baseline levels of the outcome variables and age (for the analyses examining number of years lived in the U.S.). For the analyses that involved years living in the U.S., significant moderation effects were interpreted by plotting the interaction, with simple slopes estimated at 1 standard deviation above and below the mean (Aiken & West, 1991).
Ethnic Matching Analyses
A chi-square test was used to examine the difference between treatment conditions for the predictor/moderator variable of ethnic matching. Multiple regression analyses were also conducted to examine ethnic matching as a predictor of treatment outcome. All analyses controlled for baseline values of the outcome measures.
All analyses were conducted on the intent-to-treat sample. Missing data were replaced using multiple imputation. Since these were exploratory analyses, we did not control for multiple statistical testing.
Results
Replicating Results with Latino-Only Subsample
As can be seen in Table 1, Latino adolescents receiving IPT-A as compared to TAU demonstrated significant improvement on all outcome measures at week 12, including the HRSD, CGAS, CGI-Improvement, CGI-Severity, and SAS-SR overall. There were no significant differences between groups for the SAS-SR subscales (although for the school and friends subscales, there were non-significant trends, F(1,47)=3.06, p=.09, and F(1,47)=3.65, p = .06, respectively).
| Outcome | IPT-A (N=28) Mean (SD) | TAU (N=22) Mean (SD) | F | df | P Value |
|---|---|---|---|---|---|
| HRSD | |||||
| Baseline | 18.2 (5.9) | 18.1 (5.4) | 7.57 | 1,47 | .008 |
| Week 12 | 7.8 (7.3) | 13.6 (8.4) | |||
| BDI | |||||
| Baseline | 20.8 (9.6) | 21.9 (9.1) | 4.82 | 1,47 | .03 |
| Week12 | 6.6 (8.5) | 12.5 (9.8) | |||
| CGAS | |||||
| Baseline | 52.5 (5.6) | 53.2 (6.7) | 6.07 | 1,47 | .02 |
| Week 12 | 67.9(12.5) | 59.6 (13.3) | |||
| CGI-S | |||||
| Baseline | 3.8 (0.8) | 3.8 (0.7) | 6.00 | 1,47 | .02 |
| Week 12 | 2.1 (1.1) | 2.9 (1.4) | |||
| CGI-I | |||||
| Baseline | 10.57 | 1,48 | .002 | ||
| Week 12 | 1.97 (0.8) | 3.1 (1.5) | |||
| SAS-SR | |||||
| Baseline | 2.9 (0.5) | 2.8 (0.6) | 6.36 | 1,47 | .02 |
| Week 12 | 2.2 (0.6) | 2.6 (0.7) |
Table 1 RESULTS OF ANALYSES REPLICATING MUFSON ET AL. (2004) WITH LATINO-ONLY SAMPLE
Pretreatment Symptoms and Functioning with Latino Only Sample
Table 2 describes demographics and participant characteristics within each treatment condition and overall for the Latino-only sample. There was a significant difference in ethnic matching between the conditions, χ2 (1, N=63)=9.17, p<.002, with more adolescents matching ethnically with their therapist in the IPT-A condition than in TAU (matched ethnicity for IPT-A, N=21, 75%; for TAU, N=6, 27.3%). Because of this, ethnic matching was not examined as a moderator of treatment condition in the subsequent analyses. No pretreatment differences were found between IPT-A and TAU conditions for place of birth (χ2(1, N=50) = .54, p = .34) or number of years lived in the U.S. for those born outside the U.S. or for those who spent some years living outside the U.S. In the IPT-A condition, mean years lived in the U.S. was 8.9, SD=3.2, and for the TAU condition it was 8.3, SD=4.6, (t(16) = − .35, p = .73). Differences in pretreatment functioning for place of birth indicated that adolescents born in the U.S. reported significantly more social adjustment problems at school (SAS-SR school subscale; M=2.53, SD=.70) than did foreign-born adolescents (M=2.05, SD=.57, t(48) =−2.27, p = .03). Differences in pretreatment functioning for years living in the U.S. showed that number of years adolescents had lived in the U.S. was negatively associated with baseline levels of social adjustment problems with family (SAS-SR family subscale; R2 = .17, β = − .53, p = .04). There were no significant differences among the other pretreatment variables based on place of birth or years living in the U.S.
| IPT (N = 28) N(%) | TAU (N = 22) N(%) | TOTAL (N = 50) N(%) | |
|---|---|---|---|
| GENDER | |||
| Male | 2 (7.1%) | 5 (22.7%) | 7 (14%) |
| Female | 26 (92.9%) | 17 (77.3%) | 43 (86%) |
| AGE (Mean, SD) | 14.7 (2.1) | 14.4 (1.6) | 14.6 (1.9) |
| PLACE OF BIRTH | |||
| Born in the U.S. | 19 (67.9%) | 17 (77.3%) | 36 (72%) |
| Foreign-Born | 9 (32.1%) | 5 (22.7%) | 14 (28.0%) |
| Born in U.S. but Lived Outside | 1 (3.6%) | 3 (13.6%) | 4 (8.0%) |
| DIAGNOSES | |||
| Major Depression | 16 (57.1%) | 13 (59.1%) | 29 (58%) |
| Dysthymic Disorder | 3 (10.7%) | 3 (13.6%) | 6 (12%) |
| Depressive Disorder NOS | 4 (14.3%) | 3 (13.6%) | 7 (14%) |
| Adjustment Disorder | 5 (17.9%) | 3 (13.6%) | 8 (16%) |
Table 2 DEMOGRAPHIC AND PARTICIPANT CHARACTERISTICS BASED ON TREATMENT CONDITION AND OVERALL FOR THE LATINO ONLY SAMPLE
Predictors of Treatment Outcome
Place of birth predicted BDI and SAS-SR adjustment scores at week 12 for school, family, overall social functioning, and global functioning. Adolescents born in the U.S. had significantly higher self-reported depres sion on BDI (R2 = .14, β=.31, p = .02) than did foreign-born adolescents at week 12. Additionally, U.S.-born adolescents demonstrated worse social functioning in school (SAS-SR: R2 = .13, β=.29, p = .04), with family (SAS-SR: R2 = .14, β=.28, p = .04), and in overall social functioning (SAS-SR: R2 = .12, β=.30, p = .04), than foreign-born adolescents. Finally, U.S.-born adolescents demonstrated worse global functioning (CGAS; R2 = .19, β= − .38, p = .005) than foreign-born adolescents at the end of acute treatment.
For the adolescents who were born or had spent part of their lives outside of the U.S., number of years spent in the U.S. did not significantly predict week 12 depression scores or any outcome measures (i.e., BDI, HRSD, SAS-SR school, family, or friends domain, CGI Improvement or Severity, or CGAS global functioning).
Adolescents who were ethnically matched with their therapist were rated significantly less severely depressed on the CGI (R2 = .12, β= − .26, p = .03), and reported significant overall improved social functioning at week 12 (SAS-SR: R2 = .15, β= –.32, p = .008) compared to adolescents who were not ethnically matched. Additionally, there was a non-significant trend for the ethnically matched adolescents to report being less depressed on the HRSD (R2 = .06, β= −.22, p = .08). Ethnic matching did not predict global functioning on the CGAS, self-reported BDI, CGI Improvement, or SAS-SR school, friend, and family functioning subscales.
Moderators of Treatment Outcome
Place of birth significantly moderated treatment condition when examining week 12 CGI depression severity (R2 = .28, β= −.64, p = .02) and improvement (R2 = .35, β= −.67, p = .01). As Figure 1 illustrates, for CGI Severity, U.S.-born adolescents were rated significantly less severely depressed at treatment end if they received IPT-A versus TAU (t(34) = −3.29, p = .002), whereas foreign-born adolescents demonstrated comparable severity levels regardless of treatment received (t(12) = .78, p = .44). These results were consistent with clinician CGI Improvement ratings. As Figure 2 shows, U.S.-born adolescents were rated significantly more improved at treatment end in IPT-A than TAU (t(34) = −4.21, p< .001), whereas foreign-born adolescents demonstrated comparable improvement regardless of treatment received (t(12) = .51, p = .61).
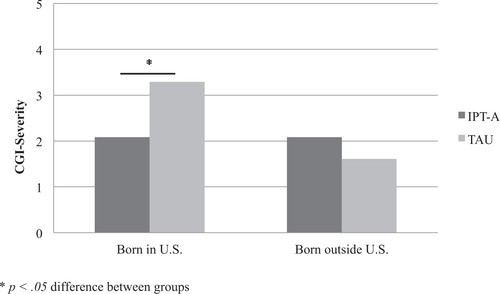
Figure 1. PLACE OF BIRTH MODERATES TREATMENT CONDITION TO PREDICT WEEK 12 CGI-SEVERITY
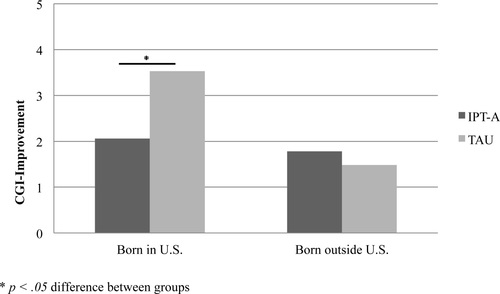
Figure 2. PLACE OF BIRTH MODERATES TREATMENT CONDITION TO PREDICT WEEK 12 CGI-IMPROVEMENT
Similar results—although with marginal significance—emerged for place of birth moderating clinician-rated depression on the HRSD (R2 = .29, β= −.47, p = .09). For the HRSD, as illustrated in Figure 3, adolescents born in the U.S. were significantly less depressed post treatment in IPT-A than TAU (t(34) = − 3.21, p = .002), whereas foreign-born adolescents demonstrated comparable depressive severity levels after treatment regardless of treatment received (t(12) = − .14, p = .89).
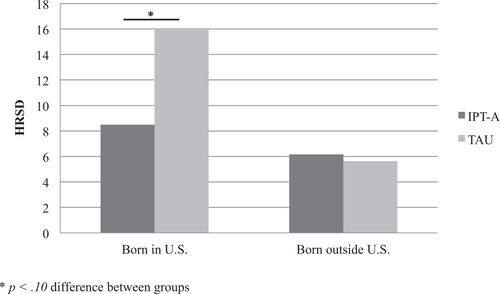
Figure 3. PLACE OF BIRTH MODERATES TREATMENT CONDITION TO PREDICT WEEK 12 HRSD
Years living in the U.S. significantly moderated treatment condition predicting overall social functioning (R2 = .36, β= −1.00, p = .04). As can be seen in Figure 4, adolescents who lived longer in the U.S. demonstrated significantly better overall social functioning post treatment in IPT-A than TAU (t(13) = −1.65, p = .01), whereas adolescents who lived fewer years in the U.S. demonstrated comparable levels of overall social functioning after treatment regardless of treatment received (t(13) = .36, p = .56).
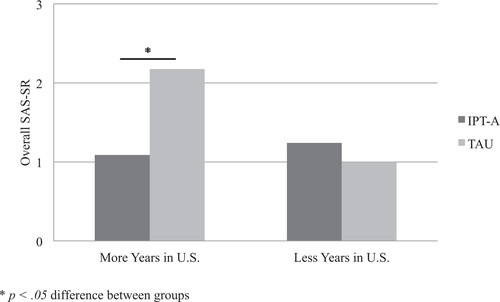
Figure 4. YEARS LIVED IN U.S. MODERATES TREATMENT CONDITION TO PREDICT WEEK 12 OVERALL SAS-SR
Discussion
This study aimed to examine the cultural responsiveness of IPT-A as compared to TAU by looking at whether level of acculturation and therapist/patient ethnic matching predicted and/or moderated treatment outcomes. First, the effectiveness of IPT-A (Mufson et al., 2004) was replicated with the Latino subsample for the major outcome measures. Next, the results suggested that greater acculturation was associated with more negative mental health outcomes for Latino youth, findings that are consistent with literature on Latino adults and adolescents (Acevedo-Garcia & Bates, 2008; Alegría et al., 2008; Peiña et al., 2008; Smokowski & Bacallao, 2007). Specifically, the study showed that prior to beginning treatment, Latino adolescents born in the U.S. reported significantly more school adjustment problems than those who were foreign-born. Amongst the adolescents who were born or spent part of their lives living outside of the U.S., greater number of years lived in the U.S. was associated with fewer pretreatment social adjustment problems within the family. Perhaps these adolescents were still more involved in their homeland customs despite the years lived in the U.S., as they tended to live in community enclaves of other Latino families and therefore faced fewer challenges to their family customs.
Findings on the acculturation proxies as moderators and predictors of treatment outcome differed between self-report and clinician-rated measures. The results suggest that for clinician-assessed outcomes, place of birth moderated the effect of treatment condition on week 12 global improvement and depressive severity (CGI), and was a marginally significant moderator of depressive symptoms (HRSD). For adolescents born in the U.S. who received IPT-A, the week 12 global depressive severity (CGI Severity Scale), global improvement of depression (CGI Improvement Scale), and HRSD depression scores were lower than for adolescents treated with usual care. Foreign-born adolescents showed no difference in week 12 global depression severity or improvement based on their CGI scores, nor were there differences in their HRSD depression scores between treatments at post-treatment. When adolescents were asked to rate their depressive symptoms and functioning, there were no differences between the treatment modalities; however, place of birth predicted depression, school, family, and overall social functioning outcomes. Adolescents born in the U.S. reported more depression symptoms (BDI), worse school, family, overall social functioning (SAS-SR), and worse global functioning (CGAS) than those foreign-born adolescents, regardless of treatment received. For those adolescents born in the U.S., the clinicians, as reported on the HRSD and the CGI Improvement and Severity Scales, perceived a benefit for the targeted depression treatment that the adolescents themselves did not recognize. Researchers have found that U.S.-born Latinos report greater perceptions of discrimination about their achievements in the U.S. as an ethnic group since immigrating, which may lead to greater levels of demoralization than for those more recent immigrants (Alegria et al., 2008; Peña et al., 2008). This sense of demoralization is possibly reflected in their more negative self-perceptions of their symptoms and functioning.
These findings suggest that level of acculturation, measured by place of birth, meaningfully affects treatment recovery for U.S.-born Latino adolescents. The immigrant paradox may help to explain these results. It states that foreign nativity protects against psychiatric disorders, although this has been shown to differ by Latino subgroups (Alegría et al., 2008). There is increasing evidence that immigrant generation status affects mental health outcomes in adult and adolescent populations (Alegría et al., 2008; Gonzales et al., 2002; Peiña et al., 2008; Smokowski, Buchanan, & Bacallao, 2009; Smokowski & Bacallao, 2007). Several models have been conceptualized to explain why U.S.-born generations have worse mental health outcomes, including 1) the protective culture model, 2) intergenerational acculturation conflict model, and 3) the resilient immigrant model (Peña et al., 2008). The current results seem most consistent with the intergenerational acculturation model, which posits that greater differences in acculturation levels between parent and adolescent create greater intergenerational conflict for more assimilated adolescents and their foreign-born parents, resulting in more emotional distress. These adolescents may have parents who are less involved in U.S. culture, resulting in a discrepancy between their acculturation and their parents’ acculturation and subsequent understanding of their host country’s (U.S.) customs and values. There is increased intergenerational conflict over issues such as curfews and dating as well as embarrassment among peers with different cultural norms. This seems consistent with other study findings that adolescents grappling with acculturation issues, parent-adolescent conflict, and perceived discrimination face an increased risk for depression and school problems (Fulgini, 1998; Smokowski & Bacallao, 2007; Vega et al., 1995).
Greater acculturative stress may also result when perceived family support does not suffice to stabilize and buffer the acculturative process (Hovey & King, 1996) as the protective culture model posits. The protective effects of Latino culture are believed to dissipate over time spent in the U.S. due to the decline in engagement in Latino culture and customs (Peña et al., 2008) and subsequent intergenerational conflict. The disengagement from their culture of origin by Latino adolescents probably exceeds that of their foreign-born parents, who are more likely to focus their social engagement within their cultural community and limit their encounters with their host country. Perhaps the Latino foreign-born youth assign more value to familismo, which may assist in their recovery from depression.
Interpersonal Psychotherapy for adolescents, with its support of the concept of familismo (Rosselló & Bernal, 1999), and its focus on targeting communication and problem-solving skills for improving relationship problems contributing to depression, may be well-suited to address the roles of enculturation and assimilation in adolescent interpersonal conflict and adjustment difficulties. This is supported by the finding that adolescents who lived in the U.S. longer reported better overall functioning at week 12 if treated with IPT-A than TAU. For those foreign-born adolescents who only had been in the U.S. for a short time, there were no differences in outcome by treatment condition. In particular, the IPT-A problem areas of interpersonal role disputes and role transitions provide specific frameworks within which to address these acculturative differences. Within this framework, the clinician can assist the adolescent in speaking with parents about cultural differences and in learning to negotiate the conflicting issues that address both parental concerns and the adolescent’s desire for assimilation. Interpersonal Psychotherapy for adolescents specifically provides the therapist with a framework for parental involvement which may not be afforded as easily by TAU. The supportive therapy provided in the TAU condition may not have specifically addressed these issues, resulting in poorer results for the U.S.-born adolescents and those grappling with greater intergenerational differences.
In the overall study sample, ethnic matching predicted significantly lower severity scores on the CGI, significantly better overall social functioning on the SAS-SR, and marginally lower HRSD depression scores at week 12. The study results indicate that ethnic matching between therapist and patient may play an important role in treatment effectiveness for reducing depression symptoms regardless of the treatment employed. As parents and other family members are frequently involved in the treatment process, parent-clinician matching may also influence outcomes for children and adolescents (Gamst et al., 2004). These findings need further exploration in a larger and more ethnically diverse sample.
Limitations
This secondary data analysis has several limitations. A primary limitation is the lack of standardized and more complex measures for assessing the influence of acculturation on treatment outcomes. In this study, length of residence in the U.S. and place of birth were proxies for acculturation. These are not ideal measures of this construct (Cabassas, 2003; Carter-Pokrasm et al., 2008; Lopez-Class et al., 2011) since they fail to examine the change processes inherent in acculturation; however, the proxies have been used in other studies of acculturation (Smokowski, Buchanan, & Bacallao, 2009; Smokowski, David-Ferdon & Stroup, 2009; Glover et al., 1999). There also were no measures of parental acculturation, which research shows may contribute to adolescents’ development of emotional problems (Smokowski, et al., 2009). Still, these analyses provide a preliminary look into the possible responsiveness of IPT-A to acculturation issues. More research needs to be done in which acculturative stress and specific changes in attitudes, beliefs, and relationships are assessed and examined as predictors and/or moderators of treatment outcome. In addition, our CGI outcome measure is a clinician rating rather than an independent evaluator rating and may be subject to bias from the clinician’s relationship with the patient.
Another limitation is the small sample size. A larger sample of adolescents with a wider range of cultural involvement (culture of origin and U.S.) and socioeconomic backgrounds might have offered greater statistical power to detect differences in outcomes between treatment conditions. We were unable to examine the effects of therapist-patient ethnic matching by treatment condition due to unequal distribution of matching across treatment conditions. Finally, we were unable to examine the effects of matching between therapist and patient language and gender on treatment outcome due to restricted variability, as most of the therapists were female (84.6%) and bilingual (76.9%). It is possible that these therapist characteristics play an important role along with ethnic matching in therapist patient-alliance and subsequent treatment outcome.
Clinical Implications
The results of this preliminary examination of the cultural competency of IPT-A for the treatment of depressed Latino youth suggest the clinical importance of assessing level of acculturation when treating Latino youth. In order to maximize the effectiveness of treatment interventions, clinicians may want to explore the factors of both enculturation and assimilation along with information regarding the adolescent’s place of birth, number of years lived in the U.S., and perception of current family values, elements that are part of the Cultural Formulation Interview (Aggarwal, Nicasio, DeSilva, Boiler, & Lewis-Fernandez, 2013). Interpersonal Psychotherapy may be particularly suited to the treatment of depressed Latino youth, especially those more highly assimilated into the United States culture. Interpersonal Psychotherapy’s close examination of the positive and negative aspects of significant relationships (interpersonal inventory) helps to identify the relationships associated with the depression, the level of support available, the stresses within the significant relationships and their contribution to or impact on the depression. The focus on current interpersonal functioning and identification of interpersonal challenges, such as role transitions and role disputes, provides a natural framework in which to address acculturation differences between the adolescent and parents as well as peers. Interpersonal Psychotherapy for adolescents also provides a framework to address perceived discrimination and associated difficulties in making the transition from country of origin to host country. The IPT-A therapist works with the adolescent to develop communication and problem-solving strategies to help navigate this new interpersonal terrain more successfully while remaining respectful of the Latino values and customs.
(2006). Toward a theory-driven model of acculturation in public health research. American Journal of Public Health, 96(8), 1342–2146.Crossref, Medline, Google Scholar
(2008).
(2013). Barriers to implementing the DSM-5 cultural formulation interview: a qualitative study. Culture, Medicine, and Psychiatry, 37, 505–533. doi:
(1991). Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage.Google Scholar
(2008). Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. American Journal of Psychiatry, 165(3), 359–369. doi:
(2006). Culture and practice: Recommendations for working with Puerto Ricans and other Latinas(os) in the United States. Professional Psychology: Research and Practice, 37(6), 694–701. doi:
(2005). Application of cultural constructs in the care of first generation Latino clients in a community mental health setting. Journal of Psychiatric Practice, 11, 221–230.Crossref, Medline, Google Scholar
(1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 8(1), 77–100. doi:
(1991). The incidence of depressive symptomatology in juvenile sex offenders with a history of abuse. Child Abuse & Neglect, 15(4), 531–536. doi:
(2001). Are empirically supported treatments valid for ethnic minorities? Toward an alternative approach for treatment research. Cultural Diversity and Ethnic Minority Psychology, 7(4), 328–342. doi:
(2006). Immigrant youth: Acculturation, identity, and adaptation. Applied Psychology, 55(3), 303–332. doi:
(1987). Further measures of the psychometric properties of the Children’s Global Assessment Scale. Archives of General Psychiatry, 44(9), 821–824. doi:
(2007). Interventions of depression symptoms among adolescent survivors of war and displacement in northern Uganda: A randomized controlled trial. Journal of the American Medical Association, 298(5), 519–527. doi:
(2003). Group interpersonal psychotherapy for depression in rural Uganda. Journal of the American Medical Association, 289, 3117–3124. doi:
(1998). Pathways to marijuana use among adolescents: Cultural/ecological, family, peer, and personality influences. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 759–766. doi:
(2003). Measuring acculturation: Where we are and where we need to go. Hispanic Journal of Behavioral Sciences, 25, 127–146. doi:
(2008). Health status of Mexican-origin persons: Do proxy measures of acculturation advance our understanding of health disparities? Journal of Immigrant Minority Health, 20, 475–488. doi:
(1991). The Hispanic stress inventory: A culturally relevant approach to psychosocial assessment. Journal of Consulting and Clinical Psychology, 3, 438–447.Crossref, Google Scholar
(2005). The well-being of immigrant Latino youth: A framework to inform practice. Families in Society: The Journal of Contemporary Social Services, 86(1), 104–111. doi:
(1995). Acculturation rating scale for Mexican American normal and clinical populations. Hispanic Journal of Behavioral Sciences, 2(3), 199–217.Google Scholar
(1990). Depressive symptoms by self-report in adolescence: Phase I of the development of a questionnaire for depression by self-report. Journal of Child Neurology, 5, 114–121. doi:
(2003). Symptom improvement and length of treatment in ethnically similar and dissimilar client-therapist pairings. Journal of Counseling Psychology, 50(1), 52–58. doi:
(1999). Drug treatment effectiveness and client-counselor empathy. Journal of Drug Issues, 29(1), 59–74.Crossref, Google Scholar
(1995). The effects of ethnicity and acculturation on early adolescent delinquency. Journal of Child and Family Studies, 4(1), 69–87. doi:
(2006). Therapist multicultural competency: A study of therapy dyads. Psychotherapy: Theory, Research, Practice, Training, 43(4), 480–490. doi:
(1998). Authority, autonomy, and parent-adolescent conflict and cohesion: A study of adolescents from Mexican, Chinese, Filipino and European backgrounds. Developmental Psychology, 34, 782–792. doi:
(2000). Ethnic match and client ethnicity effects on global assessment and visitation. Journal of Community Psychology, 28(5), 547–564. doi:
(2004). Ethnic match and treatment outcomes for child and adolescent mental health center clients. Journal of Counseling & Development, 82(4), 457–465. doi:
(1988). Recurrent depression in adolescents: A follow-up. Journal of the American Academy of Child & Adolescent Psychiatry, 27(1), 49–54. doi:
(1999). Anxiety symptomatology in Mexican-American adolescents. Journal of Child and Family Studies, 8(1), 47–57.Crossref, Google Scholar
(2004).
(2002). Acculturation and the mental health of Latino youths: An integration and critique of the literature. Westport, CT: Praeger Publishers.Google Scholar
(1976).
(2001). Psychotherapy research with ethnic minorities: Empirical, ethical, and conceptual issues. Journal of Consulting and Clinical Psychology, 69(3), 502–510. doi:
(2002). Counselor-client matching on ethnicity, gender and language: Implications for counseling school-aged children. North American Journal of Psychology, 4(3), 367–380.Google Scholar
(2005). Caregiver-therapist ethnic similarity predicts youth outcomes from an empirically based treatment. Journal of Consulting and Clinical Psychology, 73(5), 808–818. doi:
(1967). Development of a rating scale for primary depressive illness. British Journal of Social and Clinical Psychology, 6(4), 278–296. doi:
(1996). Acculturative stress, depression, and suicidal ideation among immigrant and second-generation Latino adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 35(9), 1183–1192. doi:
(2008). Evidence-based psychosocial treatments for ethnic minority youth. Journal of Clinical Child & Adolescent Psychology., 37(1), 262–301. doi:
(1998). Effect of ethnic matching of young clients and mental health staff. Cultural Diversity and Mental Health, 4(4), 297–302. doi:
(2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59, 877–884.Crossref, Medline, Google Scholar
(2006). Making the case for selective and directed cultural adaptations of evidence-based treatments: Examples from parent training. Clinical Psychology Science and Practice, 13, 295–310. doi:
(2011). Conceptions of acculturation: A review and statement of critical issues. Social Science & Medicine, 72, 1555–1562.Crossref, Medline, Google Scholar
(2013). A new measurement of acculturation for Hispanics: The Bidimensional Acculturation Scale for Hispanics (BAS). Hispanic Journal of Behavioral Sciences, 35, 486–509. doi:
(2009). Towards an adaptation of interpersonal psychotherapy for depressed Hispanic patients. Journal of Clinical Psychiatry, 70, 214–222.Crossref, Medline, Google Scholar
(2000). An exploratory study of ethnicity and psychotherapy outcome among HIV-positive patients with depressive symptoms. Journal of Psychotherapy Practice and Research, 9, 226–231.Medline, Google Scholar
, Interpersonal Psychotherapy for Depressed Adolescents, 2nd ed. New York: The Guilford Press, 2004.Google Scholar
(2004). A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry, 61, 577–584. doi:
(1999). Efficacy of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry, 56(6), 573–579. doi:
(1979). Acculturation. A psychometric perspective. American Psychologist, 34(11), 1061–1070.Google Scholar
(1992). Community mental health services for Hispanics: A test of the culture compatibility hypothesis. Hispanic Journal of Behavioral Sciences, 14(4), 455–468. doi:
(2006). Acculturation, parent-adolescent conflict, and adolescent adjustment in Mexican American families. Family Process, 45(1), 75–86. doi:
(2010). Effectiveness of an intervention led by lay health counselors for depressive and anxiety disorders in primary care in Goa, India (MANAS): A cluster randomized controlled trial. Lancet, 376(9758), 2086–2095. PMID: 21159375Crossref, Medline, Google Scholar
(2008). Immigration generation status and its association with suicide attempts, substance use, and depressive symptoms among Latino adolescents in the USA. Prevention Science, 9(4), 299–310. doi:
(2001). Legacies: The story of the immigrant second generation. University of California Press.Google Scholar
(1981). Expectations and preferences for counselor race and their relation to intermediate treatment outcomes. Journal of Counseling Psychology, 28(1), 40–46. doi:
(1999). Efficacy of cognitive-behavioral and interpersonal treatments for depression in Puerto Rican adolescents. Journal of Counseling and Clinical Psychology, 67(5), 734–745. doi:
(1996). The effects of therapist-client ethnic match in the assessment of mental health functioning. Journal of Cross-Cultural Psychology, 27(5), 598–615. doi:
(1983). A children’s global assessment scale (CGAS). Archives of General Psychiatry, 40(11), 1228–1231. doi:
(2007). Acculturation, internalizing mental health symptoms and self-esteem: Cultural experiences of Latino adolescents in North Carolina. Child Psychiatry & Human Development, 37, 273–292. doi:
(2009). Acculturation and adjustment in Latino adolescents: How cultural risk factors and assets influence multiple domains of adolescent mental health. Journal of Primary Prevention, 30, 371–393. doi:
(2009). Acculturation and violence in minority adolescents: A review of the empirical literature. Journal of Primary Prevention, 30, 215–263. doi:
(1981). Utility of the Beck Depression Inventory with psychiatrically hospitalized adolescents. Journal of Consulting and Clinical Psychology, 49(3), 482–483.Crossref, Medline, Google Scholar
(1991).
(1998). In search of cultural competence in psychotherapy and counseling. American Psychologist, 53(4), 440–448. doi:
(1991). Community mental health services for ethnic minority groups: A test of the cultural responsiveness hypothesis. Journal of Consulting and Clinical Psychology, 59, 533–540. doi:
(2006).
(1984). Race of counselor, client sex, cultural mistrust level, and premature termination from counseling among Black clients. Journal of Counseling Psychology, 31(3), 371–375. doi:
(1991). Cultural diversity and treatment of children. Journal of Consulting and Clinical Psychology, 59(6), 799–812. doi:
(2009). Defining and measuring acculturation: a systemic review of public health studies with Hispanic Populations in the United States. Social Sciences & Medicine, 69(7), 983–991.Crossref, Medline, Google Scholar
(1995). Cultural conflicts and problem behaviors of Latino adolescents in home and school environments. Journal of Community Psychology, 23, 167–179. doi:
(1988). Mistrust level and its effects on counseling expectations in Black client-White counselor relationships: An analogue study. Journal of Counseling Psychology, 35(2), 194–197. doi:
(1989). Cultural mistrust and its effects on expectational variables in Black client-White counselor relationships. Journal of Counseling Psychology, 36(4), 447–450.Crossref, Google Scholar
, (2002). Community clinic treatment of depressed youth: Benchmarking usual care against CBT clinical trials. Journal of Consulting and Clinical Psychology, 70(2), 299–310. doi:
(1976). Assessment of social adjustment by patient self-report. Archives of General Psychiatry, 33(9), 1111–1115.Crossref, Medline, Google Scholar
(2001). A comparison of three scales for assessing social functioning in primary care. American Journal of Psychiatry, 158(3), 460–466.Crossref, Medline, Google Scholar
(1980). Children’s symptom and social functioning self-report scales. Comparion of mothers’ and children’s reports. Journal of Nervous and Mental Diseases, 168, 736–740.Crossref, Medline, Google Scholar
(2013). Performance of evidence-based youth psychotherapies compared with usual clinical care: A multilevel analysis. JAMA Psychiatry, 70(7), 750–761. doi:
(1988). A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry, 45(8), 742–747.Crossref, Medline, Google Scholar
(1991). Primary prevention of acculturative stress among refugees: Application of psychological theory and practice. American Psychologist, 46(6), 632–641.Crossref, Medline, Google Scholar
(1994). Children and adolescents in community mental health centers: Does the ethnicity or the language of the therapist matter? Journal of Community Psychology, 22, 153–163. doi: